Watch following video to see demo of TUS machine
Please click on following page to order TUS device

Transcranial Ultrasonic Brain Stimulation (TUS): A New Era of Non-Invasive Neuromodulation
Transcranial ultrasonic brain stimulation (TUS) is an exciting and rapidly evolving non-invasive neuromodulation technique that utilizes focused sound waves to precisely influence brain activity. Unlike traditional methods that rely on electrical currents or magnetic fields, TUS offers unique advantages in terms of spatial resolution and the ability to target deep brain structures with unprecedented accuracy. This detailed article explores the indications, mechanism of action, typical dose and frequency parameters, potential side effects, and promising clinical results of TUS.
Indications: Expanding Therapeutic Frontiers
TUS is currently a subject of intense research for a wide array of neurological and psychiatric conditions, with promising early results in many areas:
Movement Disorders: While high-intensity focused ultrasound (HIFU) is already FDA-approved for ablative treatments of essential tremor and Parkinson’s tremor, low-intensity TUS is being investigated for non-ablative neuromodulation to improve various motor symptoms in Parkinson’s disease, dystonia, and other movement disorders.
Psychiatric Conditions: TUS shows significant promise for:
Depression: Research is exploring TUS to modulate brain regions implicated in mood regulation, such as the prefrontal cortex and deeper limbic structures.
Obsessive-Compulsive Disorder (OCD): Similar to depression, TUS is being investigated for its potential to alter activity in dysfunctional brain circuits associated with OCD.
Anxiety Disorders: Early studies are exploring TUS for generalized anxiety and other anxiety-related conditions.
Substance Use Disorders: TUS is being explored as a potential treatment to modulate reward pathways and craving.
Neurological Conditions: Alzheimer’s Disease and Dementia: TUS is being explored not only for direct neuromodulation to improve cognitive function but also for its ability to temporarily open the blood-brain barrier (BBB), facilitating the delivery of therapeutic agents to the brain.
Epilepsy: TUS could potentially be used to suppress abnormal neural activity in seizure-generating regions.
Autism, Aphasia, ADHD
Chronic Pain: By targeting specific pain processing centres in the brain, TUS aims to provide relief from chronic neuropathic pain.
Stroke Rehabilitation: TUS may enhance neuroplasticity and recovery of function after stroke.
Disorders of Consciousness: Emerging research suggests TUS could help improve consciousness in patients with vegetative states or minimally conscious states by stimulating deep brain structures like the thalamus.
Mechanism of Action: The Biophysics of Sound in the Brain
The precise mechanisms by which TUS modulates neural activity are still under active investigation, but a growing body of evidence points to several key biophysical effects:
Mechanical Deformation of Neuronal Membranes: Ultrasound waves are mechanical vibrations that induce minute pressure changes and mechanical stress on neuronal cell membranes. This deformation can directly influence the opening and closing of mechanosensitive ion channels (e.g., Piezo channels, TREK-1). Changes in ion flow (e.g., calcium influx) can then alter membrane potential, leading to depolarization (excitation) or hyperpolarization (inhibition) of neurons.
Acoustic Streaming and Radiation Force: The propagation of ultrasound waves through tissue can induce acoustic streaming (fluid movement) and radiation force (a steady force exerted by the wave). These phenomena can exert shear stress on cell membranes and alter the microenvironment around neurons, potentially influencing neurotransmitter release, synaptic plasticity, and metabolic activity.
Micro cavitation (Stable): At low intensities, ultrasound can induce stable cavitation, where microscopic gas bubbles naturally present in tissue or intentionally introduced (e.g., microbubbles for BBB opening) oscillate without collapsing. These oscillating bubbles can create localized mechanical effects and enhance the interaction of ultrasound with neural tissue. Unstable (inertial) cavitation, which can cause tissue damage, is typically avoided in neuromodulator TUS protocols.
Thermal Effects (Minimal for Neuromodulation): While high-intensity focused ultrasound (HIFU) used for ablation relies on significant temperature increases to destroy tissue, neuromodulator TUS typically operates at low intensities designed to minimize thermal effects. Any subtle temperature changes that occur are thought to be secondary to the primary mechanical effects and are generally below the threshold for tissue damage.
Influence on Glial Cells and Neurovascular Coupling: TUS may also indirectly influence neural activity by affecting glial cells (astrocytes, microglia) and modulating neurovascular coupling, thereby altering local blood flow and nutrient supply to neurons.
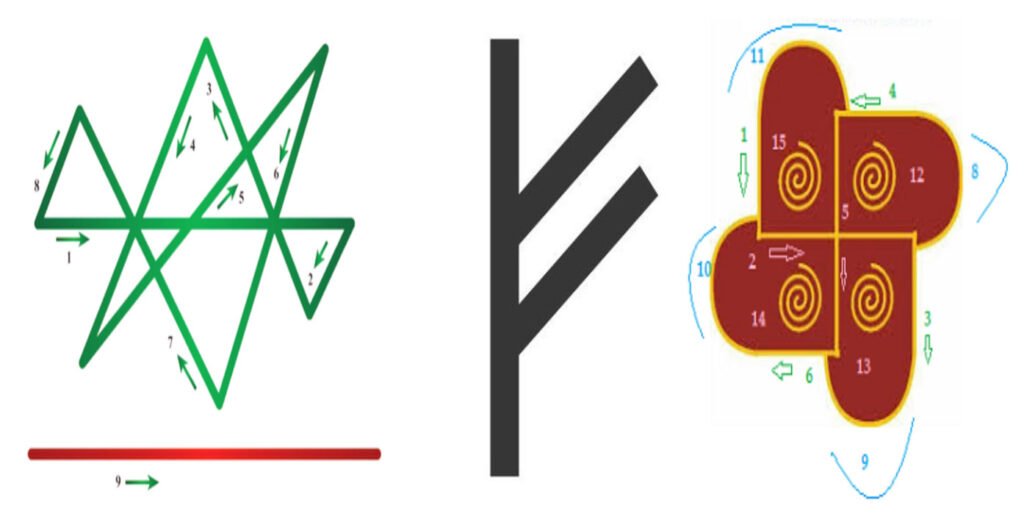
The ability of TUS to induce both excitatory and inhibitory effects on neural activity is thought to be dependent on the specific acoustic parameters used, including frequency, intensity, pulse repetition frequency, and sonication duration.
Dose, Duration, and Frequency: Optimizing the Acoustic Profile
Optimizing TUS parameters is crucial for achieving desired therapeutic effects while ensuring safety. Research is continually refining these parameters, but general guidelines are emerging:
Frequency: Most neuromodulator TUS applications use frequencies ranging from 250 kHz to 1 Megahertz. Lower frequencies (e.g., 0.5 MHz) offer better skull penetration and can reach deeper brain structures, while higher frequencies provide finer spatial resolution.
Intensity: TUS for neuromodulation operates at low intensities, typically with a spatial-peak pulse-average intensity (I SPPA) often below 1-3 W/cm² and a spatial-peak temporal-average intensity (I SPTA) typically below 3 W/cm². These intensities are significantly lower than those used for ablative procedures (HIFU), minimizing thermal effects.
Pulse Repetition Frequency (PRF): The rate at which individual ultrasound pulses are delivered. PRF can range from 10 Hz to 2 kHz, and plays a critical role in determining the type and magnitude of neural response.
Duty Cycle (DC): The percentage of time the ultrasound is actively “on” within a pulse cycle. Low duty cycles (e.g., <50%, often 1-10%) are commonly used to prevent excessive heating.
Sonication Duration: The length of time an individual ultrasound burst is applied. This can range from milliseconds to several seconds.
Treatment Duration and Frequency: Protocols vary widely depending on the condition and research aims. Some studies involve single sessions, while others involve multiple daily or weekly sessions over several weeks or months. For example, some protocols for cognitive enhancement or depression might involve 10-30 sessions.
Precise targeting of brain regions is achieved using neuroimaging techniques like MRI (magnetic resonance imaging) to create personalized treatment plans, often guided by neuronavigational systems.
Side Effects: A Generally Safe Profile
Transcranial ultrasonic brain stimulation is considered safe, especially when applied at low intensities. Most reported side effects are mild and transient, typically resolving within minutes to hours or days.
Common (Mild and Transient): Headache/Head Pain: The most frequently reported side effect.
Scalp Sensation: Tingling, warmth, or pressure sensation at the site of stimulation.
Dizziness/Light-headedness: Can occur during or shortly after stimulation.
Fatigue: Some individuals may experience temporary tiredness.
Nausea: Less common, but possible.
Auditory Sensations: Although ultrasound is above the human hearing range, some individuals may perceive faint sounds or clicks due to bone conduction.
Minor Skin Redness/Irritation: At the application site.
Mood Changes/Anxiety: Transient alterations in mood.
Cognitive Issues: Very rare and usually transient.
Safety protocols, including strict adherence to acoustic intensity limits and continuous monitoring, are paramount to minimize risks.
Results: Promising Efficacy and Future Directions
The results from preclinical and early clinical studies of TUS are highly encouraging:
Modulation of Neural Activity: Studies have consistently shown that TUS can non-invasively excite or inhibit specific neural circuits in both superficial and deep brain regions, as evidenced by changes in electroencephalography (EEG), functional MRI (fMRI), and behavioural responses.
Cognitive Enhancement: Several studies have demonstrated TUS-induced improvements in memory, attention, and executive functions in healthy individuals and patients with cognitive deficits (e.g., Alzheimer’s disease).
Symptom Reduction in Psychiatric Disorders: Preliminary trials have reported reductions in symptom severity for treatment-resistant depression, OCD, and chronic pain, though larger, placebo-controlled trials are needed to confirm these effects.
Motor Function Improvement: TUS applied to motor areas has shown the ability to induce and modulate motor-evoked potentials and improve motor performance.
Blood-Brain Barrier Opening: TUS, often combined with intravenously injected microbubbles, has been successfully used to temporarily and focally open the BBB in humans, allowing for enhanced delivery of therapeutic agents (e.g., antibodies, chemotherapy) to target regions, which is a major breakthrough for treating brain tumours and neurodegenerative diseases.
Neuroplasticity Induction: TUS has been shown to induce long-lasting changes in synaptic plasticity, suggesting its potential for therapeutic applications requiring durable alterations in brain circuits.
As the understanding of TUS mechanisms deepens and technological advancements enable even more precise and versatile applications, transcranial ultrasonic brain stimulation holds immense potential to revolutionize the treatment of a wide range of neurological and psychiatric conditions, offering a highly precise, non-invasive, and well-tolerated therapeutic option.